
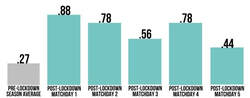
However, science tells us not to rush. Science tells us that training in a structured way may actually prevent against injury but excessive and rapid increases in training loads are likely responsible for a large proportion of non-contact, soft-tissue injuries (Gabbett, 2016). It’s the latter part of that statement that worries me, particularly in the return to sport environment we all now find ourselves in. While trawling through Twitter recently I came across the trackademic blog that referenced the below graphic. I did lose sleep over it. It’s from a study of the return of the Bundesliga and the injury rates in matches since that return. These guys are professional athletes with every resource under the sun available to them. I’m presuming they had decent levels of fitness pre-covid and resources to at least maintain during the enforced off season. It’s definitely a statistic to chew on/cry over and plan for in your upcoming re championship training.




 RSS Feed
RSS Feed
